This thinking ignores that there is already significant overlap between the criminal-justice system and the mental-health system. The further intermingling of these systems could very well end badly both for people who are imprisoned and people who are receiving psychiatric treatment.
Despite calls from prison-reform activists for more diversion to treatment for those who are jailed, the lives of those involuntarily committed to treatment for mental illness are subject to judicial intervention from the start of their confinement in one of the designated facilities in the state.
They are subject to court orders that allow them to be drugged forcibly and orders of non-hospitalization that require that they take psychiatric drugs once they are out of the hospital setting, lest they be returned to the hospital.
They face months of involuntary confinement, at the discretion of a judge.
An added emphasis on mental-health care in the criminal-justice system is less likely to result in an increase in meaningful counseling and compassionate care, and it could easily result in the increased use of antipsychotics as a means of chemical restraint.
There is also likely to be an additional layer of surveillance once inmates are released on parole or probation. In this scenario, inmates may be freed on the condition that they adhere to a regime of medication that may not be needed and that may be ultimately harmful to their physical or mental health.
This is not to say that there are not unmet needs among the imprisoned, and that drastic changes are not required to address these needs.
The Vermont Department of Corrections reported that in 2015 that 47 percent of those imprisoned were receiving mental-health services. According to the Vermont Human Rights Commission, there are obvious dangers attendant with this already-established relationship — particularly an increased reliance on solitary confinement.
To equate crime and untreated mental illness without explanation or qualification also serves to obscure criticisms of both the criminal-justice and the mental-health systems. It provides a pat set of explanations and solutions to social problems that require a more-thorough examination.
In accepting these explanations and solutions, we lose perspective on both and gain nothing in terms of public safety or the preservation of human rights.
Essentially, this puts the cart before the horse: being imprisoned is a traumatic experience that in many cases precipitates emotional crises.
In a 2017 report, the U.S. Bureau of Justice Statistics reported that some 1 in 7 prison inmates and 1 in 4 jail inmates reported serious psychological distress in the 30 days preceding a 2011-2012 survey.
While it would be possible to infer the harmful stereotype that many prisoners are mentally ill (and that many who experience mental illness are incipient prisoners), it is more politically astute to argue that losing one’s freedom and being placed in an institutional setting leads to emotional crises.
The same argument can be made for involuntary admission to a mental hospital, where patients experience many of the same losses of freedom.
In a report to the Department of Mental Health, Wilda White, executive director of Vermont Psychiatric Survivors notes that homelessness is the most significant determinant of long wait times in an emergency department. Housing status is also a major predictor of who will come into contact with the police.
Homelessness, incarceration, and civil commitment are all interrelated and mutually reinforcing phenomena that have economic inequality at their base rather than mental illness.
The way forward is not continuing to warehouse those who are suffering, but to redirect funding to housing and other programs that provide people with resources for survival.
In a 2016 report, the Center for American Progress estimated that the costs associated with providing supportive housing to inmates who are disabled is half of what it costs to incarcerate them.
While the proposed facility in Franklin County represents a commingling of the worst impulses that accompany calls for increased public safety and increased treatment for mental illness, it brings us opportunities for increased collaboration between prison reform and abolition movements and the movements of psychiatric survivors.
If the $3.25 billion that this mega-prison is anticipated to cost over 20 years were to be allocated to the development of truly affordable and accessible housing, we would more effectively address the issues that psychiatric hospitalization and imprisonment purport to solve.
And at the same time, we would forego the loss of freedom, exacerbation of suffering, and perpetuation of stigma that they actually deliver.
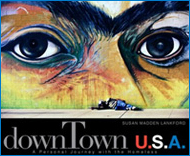
© Humane Exposures / Susan Madden Lankford